Antibiotics And Probiotics: Definition, Best Strains And Timing
Antibiotics are a class of medications that inhibit the growth or destroy bacteria, effectively treating bacterial infections in humans and animals. In 2013, almost 67 million children under 19 in the US were prescribed Antibiotics according to the CDC.
Unlike antibiotics, probiotics are beneficial bacteria intended to improve digestive health and overall well-being. Probiotics are live microorganisms, such as bacteria or yeasts, that, when ingested in adequate amounts, confer health benefits on the host by promoting a balanced gut microbiome.
What Are Antibiotics?
Antibiotics are medications used to treat or prevent bacterial infections.
They work by killing bacteria or preventing their growth and reproduction. Antibiotics are not effective against viral infections such as the common cold or flu. They are prescribed by doctors and are important for treating serious bacterial infections, although some mild bacterial infections can get better on their own without antibiotics. It is crucial to use antibiotics only when necessary to prevent antibiotic resistance and to avoid potential side effects.
Common side effects of taking antibiotics include diarrhea, nausea, vomiting, dizziness, rash and yeast infections. These side effects are usually mild and temporary, and they tend to resolve once the course of antibiotics is completed. More serious side effects can occur, such as Clostridioides difficile infection which is a bacterial infection that can cause severe diarrhea and inflammation of the colon.
How Are Antibiotics Made?
Antibiotics are typically produced through a process called fermentation in industrial microbiology.
During fermentation, the source microorganism responsible for producing the antibiotic is grown in large containers containing a liquid growth medium. Various factors such as oxygen concentration, temperature, pH, and nutrients are closely controlled during this process.
Antibiotics are often derived from soil microorganisms and are a product of their secondary metabolic pathways. These pathways utilize common metabolites in specific and intricate ways to produce antibiotics. The fermentation process allows for the large-scale production of antibiotics for medical use.
What Is Antibiotic Resistance?
Antibiotic resistance refers to the ability of bacteria and fungi to develop mechanisms that allow them to withstand the effects of antibiotics.
Antibiotic resistance occurs when these microorganisms change in response to the use of antibiotics, making the drugs ineffective in killing or inhibiting their growth. This resistance can be acquired through various mechanisms, including genetic mutations and the transfer of resistance genes between bacteria.
Antibiotic resistance poses a significant threat to public health as it can lead to more difficult-to-treat infections, increased healthcare costs, and higher mortality rates according to WHO. Efforts to combat antibiotic resistance involve promoting appropriate antibiotic use, developing new antibiotics, and implementing infection prevention and control measures according to a 2020 study authored by MAA Majumder.
Do Antibiotics Kill Good Bacteria In Your Gut?
Yes, antibiotics kill good bacteria in your gut negatively affecting the gut microbiome according to research.
A 2022 study authored by DV Patangia, found that the gut microbiota plays a crucial role in host health, and antibiotic use can disrupt the microbial balance and negatively impact host health.
Antibiotics can lead to reduced microbial diversity, changes in the functional attributes of the microbiota, and the formation of antibiotic-resistant strains, making hosts more susceptible to infections like Clostridioides difficile. The study emphasizes the need for careful antibiotic stewardship, exploring alternative approaches to antibiotic use, and developing methods to conserve and restore the microbial community after antibiotic-associated perturbations.
Can You Take Probiotics With Antibiotics?
Yes, you can take probiotics with antibiotics and it is beneficial to take probiotics alongside antibiotics.
Taking probiotics alongside antibiotics can help restore beneficial bacteria in the gut that may be affected by antibiotic treatment. It is recommended to wait at least two hours after taking antibiotics before taking probiotics to prevent the antibiotic from killing the beneficial bacteria in the probiotic supplement. It is advisable to choose high-quality probiotics from a trusted source if opting to take them with antibiotics.
Best Probiotic For Antibiotics?
The 4 best probiotics for antibiotics are Lactobacillus rhamnosus GG, Lactobacillus Acidophilus, Saccharomyces boulardii and Bifidobacterium lactis CCT 7858 according to research.
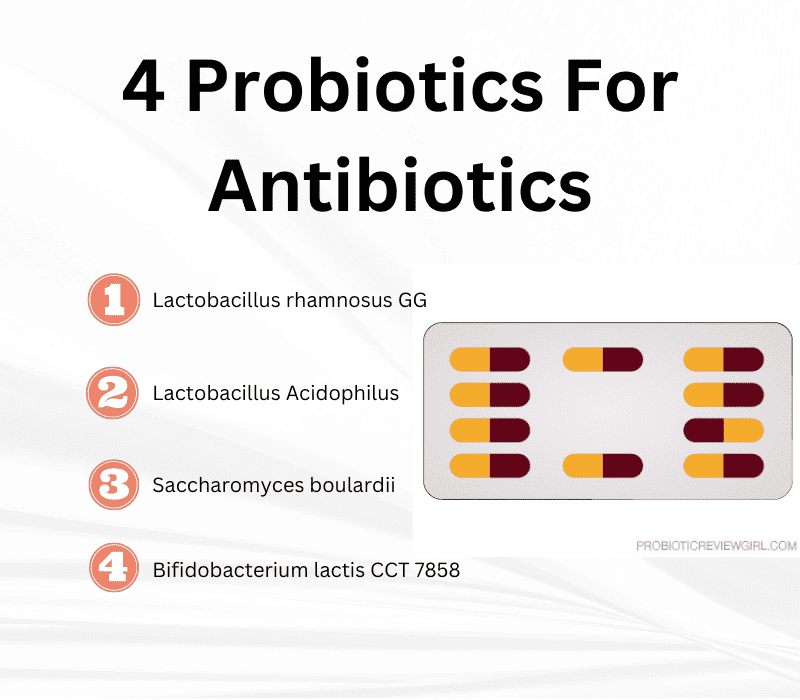
- 1Lacotbacillus Rhamnosus GG: A 1999 study authored by JA Vanderhoof, found that this strain an effectively reduce the incidence of antibiotic-associated diarrhea in children receiving oral antibiotics for common childhood infections. In a double-blind randomized trial, children who received LGG alongside their antibiotic therapy had a significantly lower incidence of diarrhea compared to those who received a placebo. LGG supplementation improved stool frequency and consistency, providing evidence for the efficacy of LGG in preventing antibiotic-associated diarrhea in children.
- 2Lactobacillus acidophilus: A 1995 study authored by DL Witsell, found that the concomitant use of Lactobacillus acidophilus with oral broad-spectrum antibiotic therapy significantly decreases patient complaints of gastrointestinal side effects and yeast superinfection. In this prospective randomized trial involving outpatients with ear, sinus, or throat infections, some of whom were receiving amoxicillin/clavulanate as the antibiotic of choice, patients were randomly assigned to either receive amoxicillin/clavulanate alone or in combination with Lactobacillus acidophilus. The patients who received Lactobacillus acidophilus reported a significant reduction in gastrointestinal side effects compared to those who received only the antibiotic.
- 3Saccharomyces boulardii: A 1995 study authored by DL Witsell, found that the concomitant use of Lactobacillus acidophilus with oral broad-spectrum antibiotic therapy significantly decreases patient complaints of gastrointestinal side effects and yeast superinfection. In this prospective randomized trial involving outpatients with ear, sinus, or throat infections, some of whom were receiving amoxicillin/clavulanate as the antibiotic of choice, patients were randomly assigned to either receive amoxicillin/clavulanate alone or in combination with Lactobacillus acidophilus. The patients who received Lactobacillus acidophilus reported a significant reduction in gastrointestinal side effects compared to those who received only the antibiotic.
- 4Bifidobacterium lactis CCT 7858: A 2023 study authored by M Michels, found that this strain at a concentration of 9 × 10^10 CFU can improve gastrointestinal symptoms and prevent diarrhea in hospitalized patients undergoing antibiotic treatment. "9 × 10^10 CFU" represents 9 multiplied by 10 raised to the power of 10 CFU. In numerical terms, this corresponds to 90,000,000,000 CFU. Patients in the Bifidobacterium lactis group (74.5%) reported no diarrhea compared to the placebo group. Secondary outcomes also showed benefits, such as a lower incidence of abdominal distension in the Bifidobacterium lactis group compared to the placebo group.
Lactobacillus acidophilus Rosell-52, Lactobacillus rhamnosus Rosell-11 and Bifidobacterium lactis Lafti B94 are some other probiotic strains that may be good for antibiotics but more clinical research is needed.
When To Take Probiotics With Antibiotics?
You should wait 1 or 2 hours after taking antibiotics before taking probiotics.
This allows for a time gap between the two medications. You can start taking probiotics on the same day as starting antibiotics, but not taking them at the exact same time. This approach aims to ensure that both medications can be effectively absorbed and utilized by the body.
There is no clear consensus on the specific timing or interval between taking probiotics and antibiotics. It may vary depending on the individual, the specific probiotic product, and the antibiotic being used. Taking probiotics alongside antibiotics can help reduce the potential damage to the gut microbiome caused by the antibiotics. Probiotics can help maintain a healthy balance of beneficial bacteria in the gut.
Should Toddlers Take Probiotics With Antibiotics?
Yes, Toddlers should take probiotics according to research to prevent side effects.
A 2020 study authored by T Yan, found that probiotics, specifically Lactobacillus rhamnosus GG and Saccharomyces boulardii, can effectively prevent antibiotic-associated diarrhea in children. The optimal dose of probiotics has not been established, but higher doses ranging from 5 to 40 billion colony-forming units per day have shown the most efficacy in trials.
Probiotics work by providing a health benefit to the host through various mechanisms, such as creating a physical barrier against pathogens, promoting mucus secretion, maintaining intestinal integrity, producing antimicrobial factors, and stimulating the immune system. The safety profile of probiotics is excellent in healthy children, although rare serious adverse events have been documented in severely debilitated or immunocompromised children.
What Is Antibiotic Associated Diarrhea?
Antibiotic-associated diarrhea (AAD) refers to the passing of loose, watery stools three or more times a day after taking medications used to treat bacterial infections, specifically antibiotics.
The exact cause of AAD is not fully understood but is commonly believed to occur when antibiotics disrupt the balance of good and bad bacteria in the gastrointestinal tract.
The risk of AAD is higher with certain antibiotics, such as aminopenicillins. Treatment and prevention strategies for AAD include discontinuing or changing the antibiotic, providing rehydration, and considering probiotics as a potential option. AAD occurs in 5-10% of patients taking antibiotics and can be managed effectively with appropriate interventions according to a 2017 study authored by S Blaabjerg.
Can Probiotics Interfere with Antibiotics?
Probiotics do not interfere with Antibiotics according to the latest research.
A 2013 study authored by B Rodgers, recommend taking probiotic supplements or consuming probiotic foods, such as yogurt or kefir, alongside a course of antibiotics. Taking probiotics alongside antibiotics is believed to help reduce damage to the gut microbiome and protect against some of the negative impacts of antibiotics on gut health.
Can Antibiotics Cause Dysbiosis?
Yes, repeated use of antibiotics can cause antibiotic-associated dysbiosis according to research. A 2023 study authored by D Kesavelu, found that antibiotic use can cause gut dysbiosis, which refers to alterations in the composition and diversity of the gut microbiota. Antibiotics not only target disease-causing bacteria but also disrupt beneficial gut microbes.
This antibiotic-associated dysbiosis is characterized by reduced diversity of the gut microbiota, changes in the abundance of certain microbial taxa, alterations in gene expression, protein activity, and gut metabolome, compromised colonization resistance to harmful bacteria, and the emergence of antibiotic-resistant microbes.
Can Probiotics Reverse Antibiotic Damage?
Yes, probiotics can reverse antibiotic dysbiosis damage on the microbiome according to research.
The same 2023 study authored by D Kesavelu, found that probiotics have the potential to prevent or reverse antibiotic-associated gut microbiota dysbiosis. The study emphasizes the importance of prudent antibiotic use among vulnerable populations, such as neonates and young children, to prevent detrimental effects on gut health caused by antibiotic-associated dysbiosis.
Can I Eat Yogurt With Antibiotics?
Yes, you can eat yogurt with antibiotics according to research.
Eating yogurt and other probiotic foods alongside antibiotics can help prevent diarrhea, reduce bloating and frequent bowel movements according to Harvard University. Probiotics provide beneficial bacteria to support digestive health and overall well-being, while antibiotics are prescribed to treat bacterial infections.
It's recommended to space out dairy product consumption from antibiotic intake by at least two to three hours to avoid interference. Consuming yogurt while on antibiotic therapy can be beneficial, but it should be taken separately from each dose of medication.
Probiotic yogurt is a dairy product containing live beneficial bacteria that can promote a healthy gut microbiome when consumed.
Dr. Sara Mesilhy has a Master’s degree in Gastroenterology and holds a membership with the Royal College of Physicians of the United Kingdom. She completed her Bachelor of Medicine, Bachelor of Surgery (MBBS) at Cairo University and is currently part of the ProbioticReviewGirl medical team.
In about to start a course of augmentin,I don’t recall it giving me any I’ll affects, but I’m prepared incase. I stocked up on florostar probiotics and yogurts. I’m not sure what you were saying about prebiotics. You barely Mentone it. Should I look to take them as well?
Hi James,
Florastor is a good Saccharomyces boulardii probiotic for helping with antibiotic-associated diarrhea. Some yogurts are a good source of Lactobacillus & Bifidobacteria. Kefir milk is another great option for a more diverse hit of strains.
You are right, Pre-biotics are very important for feeding probiotic bacteria. You can get them easily through a daily diet with things like dark leafy greens, asparagus, and others provided they are not over-cooked. My probiotic FlowFlora also includes a FOS prebiotic fiber. Good luck 🙂
Hi, kam dashur te di cmimin tuaj